Frequently need to pee? App-based therapy can help, finds research
Combining pelvic floor exercises with behavioral therapy could be more effective than current medical treatments at helping men with frequent urges to urinate, new research in men has found.

Oral vaccine for UTI is potential alternative to antibiotics, finds 9-year study
Recurrent Urinary Tract Infections (UTIs) can be prevented for up to nine years in more than half of people given an oral spray-based vaccine and is a potential alternative to antibiotic treatments, finds research.

Urine test halves painful procedures in bladder cancer follow up, new trial shows
A simple urine test can more than halve the number of cystoscopies necessary to follow up high-risk bladder cancer patients, new research has found.
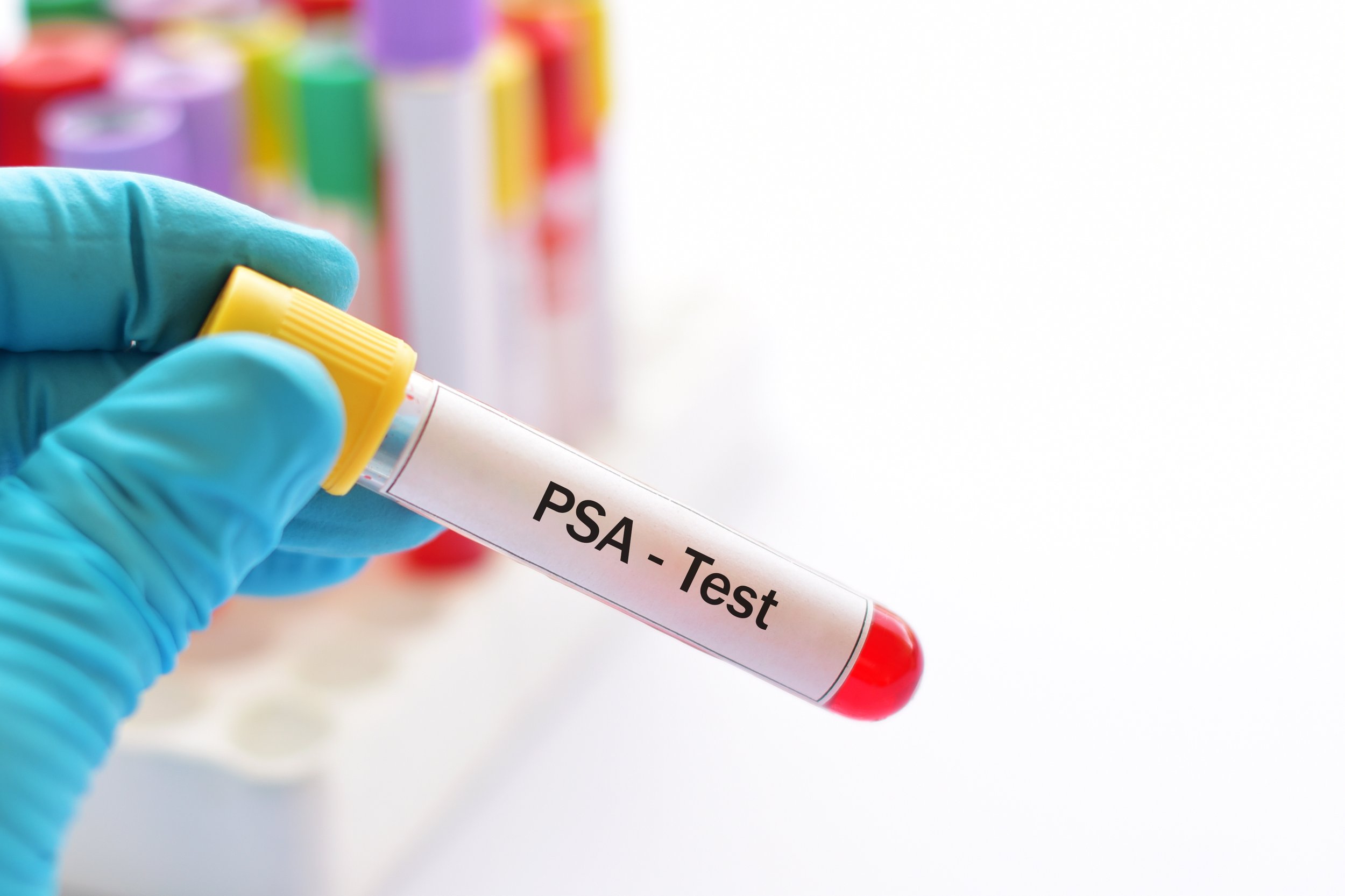
Five-year interval is safe for prostate cancer screening, research shows
A simple blood test every five years is sufficient to screen low risk men for prostate cancer, new research has shown.

Bladder cancer treatment can be better targeted and more effective, trials show
Testing for tumour DNA in the blood can successfully identify advanced bladder cancer patients who will not relapse following surgery, new research shows.